Pharmacotherapy/Treatment Of Eye Infection
The eye is the organ of sight. Some say it is the most important organ of the body. The word "eye" comes from the Teutonic "auge." The eye has a number of components. These components include but are not limited to the cornea, iris, pupil, lens, retina, macula, optic nerve, choroid and vitreous.
Eye Anatomy
The anatomy of the eye is complex. The main structures of the eye include:
Cornea: clear tissue in the very front of the eye
Iris: colored part of the eye surrounding the pupil
Pupil: dark hole in the iris that regulates the amount of light going into the eye
Lens: small clear disk inside the eye that focuses light rays onto the retina
Retina: layer that lines the back of the eye, senses light, and creates electrical impulses that travel through the optic nerve to the brain
Macula: small central area in the retina that allows us to see fine details clearly
Optic nerve: connects the eye to the brain and carries the electrical impulses formed by the retina to the visual cortex of the brain
Vitreous: clear, jelly-like substance that fills the middle of the eye
Eye Infection
Eye Infection occurs when harmful microorganisms invade any part of the eyeball or surrounding areas. Microorganisms include bacteria, parasites, fungi and viruses. These organisms can invade the clear front surface of the eye (cornea) and the thin moist membrane lining the outer and inner eyelids (conjunctiva).
Read Also: Pharmacotherapy/Treatment Of Fungi Skin infection
Symptoms
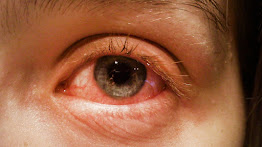
1. Red eyes
2. Pain in the eyes
3. Eye discharge
4. Dry eyes
5. Watery eyes
6. Photophobia light sensitivity
7. Swelling around the eyes
8. Itchy eyes
9. Blurring vision
10. Swollen eyes
Diagnosis
There are many types of eye infection. There are many ways to diagnose different types of infection. A medical doctor takes a patient's history and other health-related information with the symptoms before deciding on which diagnosis will be right to predict the type of eye infection.
Using a solution put into the eyes to dilate it for examination is the most common way to diagnose eye infection. Eye discharge can be sent to the laboratory for analysis.
Pink Eye (Conjunctivitis)
Pink eye otherwise known as conjunctivitis is an infection that affects the conjunctivitis. It makes the eye look pink.
 |
| Conjunctivitis (pink eye) Image gallery |
Symptoms
1. Redness in the white of the eyes or inner eyelids
2. Swollen conjunctiva
3. Thick yellow discharge that crust over the eyelashes especially after sleep
4. More tears than usual
5. Green or white discharge from the eyes
6. Itchy eyes
7. Burning eyes
8. Blurred vision
9. Photosensitive
10. Swollen lymph nodes often from viral infection
11. It can make the eye stick together after waking up
Cause
Pink eyes also known as conjunctivitis is caused by virus, fungi, parasites, bacteria, irritant or allergic reactions. It is very common in cold infection. Pink eye in children is usually caused by bacteria whereas that of adults is usually caused by a virus.
Pink eyes are very contagious. However, it is not really dangerous especially when the treatment is started on time. Gonorrhea and chlamydia are very common infections that cause pink eyes and can be dangerous if not treated on time.
Diagnosis
Diagnosis is using different techniques to check for visual acuity. That is if the eye can still see clearly. Further investigation requires examination of the eye with a slit lamp. A fluorescein is dropped inside the conjunctival sac and the eye is viewed with the aid of cobalt blue light or slit lamp or fundoscore is done to rule out any signs of corneal ulceration or infection.
Types
Classification is based on the cause of the conjunctivitis.
Viral Conjunctivitis
This is the most common conjunctivitis. It is more prevalent in adults than children.
Symptoms
They tend to start from one eye where they cause loss of tears and a watery discharge from the eyes. Within a few days, the other eye gets involved. Could feel a swollen lymph node in front of the ear or under the jaw bone. The whole symptom is as a result of a dilation of the conjunctival blood vessels resulting in inflammation.
Cause
Adenovirus is responsible for 65-90 percent of viral conjunctivitis. Others are herpes simplex virus and zoster virus.
Pharmacotherapy/Treatment
Viral conjunctivitis is self limiting. There is no specific treatment. Medical intervention is management of symptoms. Cold compress 3-4 times a day helps to suppress pain and inflammation. That can be applied until symptoms go away. Artificial tears may be necessary when the eyes are itchy and dry. Antihistamine topical and oral can help with serious itch. Acyclovir ointment and ganciclovir gel may be necessary for herpes simplex virus and zoster virus.
Bacteria Conjunctivitis
This is more common in children
Cause
Commonly caused by haemophilus influenzae, streptococcus pneumoniae and streptococcus aureus.
Symptoms
Appear as pus or mucus in one or both eyes.
Pharmacotherapy/Treatment
Treatment involves the use of one of the following antibiotic eye preparations.
1. Chloramphenicol 0.5% eye drop 1-2 drops in both eyes every 2 hours for the first 24 hours then subsequently every 6 hours for another 6 days.
2. Framycetin sulphate 0.5% eye drop 1-2 drops on both eyes every 1-2 hours for the first 24 hours then subsequently 8 hourly for 6 days.
3. Chloramphenicol eye ointment at bedtime
Gentamicin, tobramycin and quinolones eye drops are not recommended for empiric treatment.
Gonococcal Conjunctivitis
This type of conjunctivitis is not very common and mostly found in infants and sexually active people.
Diagnosis
Gram staining and special culture for neisseria.
Pharmacotherapy/Treatment
The eye is lavage with saline water morning and night and ceftriaxone injection given according to the recommended dose.
Chlamydia Conjunctivitis
They appear as unilateral and it affects people suffering from genital infection concurrently.
Symptoms
1. Conjunctiva hyperaemia
2. Mucopurulent discharge
3. Lymphoid follicle formation
Pharmacotherapy/Treatment
It is very easy to treat. Oral azithromycin and doxycycline taken at the right dose.
Ophthalmia Neonatorum
Is a serious form that affects newborn babies. It is caused by a bacteria.
Management
During treatment, it is best to always clean the eyes to make the healing process fast. Also, it is wrong to use the same pillowcase every other night. Infected eyes should not be touched with bare hands to avoid spreading it to the other eyes or reinfection. Sharing glasses is a bad habit that can prevent the healing process. Wearing glasses help protect the eyes from external light which can be painful and dust. Lastly, the use of eye patches should be avoided.
Cytomegalovirus (CMV) Retinitis
Cytomegalovirus (CMV) Retinitis is an eye infection that attacks the eye sensing cell in the retina. It is more common in women than in men. It appears in one eye and overtime spreads to the other.
Symptoms
1. Floaters in the eyes
2. Blurred spot
3. Blurred vision
4. Loss of peripheral vision
5. Flashes in the eye
Causes
It is caused by cytomegalovirus (CMV). CMV occurs in several parts of the body. It is more common in the skin and retina. It lies dormant in the body and resurfaces when the body immune system is down. The major cause of weakened immune systems related to CMV infection is human immunodeficiency virus/acquired immune disease syndrome (HIV/AIDS). It used to affect more than 80 percent of HIV/AIDS patients but recent advancements in treatment have reduced this figure. Other causes are drugs, chemotherapy, disease, newborn, erderly and organ transplant surgery.
Pharmacotherapy/Treatment
The first step is to strengthen the immune system. Subsequently, intravenous ganciclovir, cidofovir and foscarnet can be given. Ganciclovir and foscarnet require an indwelling catheter placed in the chest for daily infusion.
Oral ganciclovir can be administered after two week of IV or intravitreal implant called vitrasert (Bausch+lomb). The implant is inserted into the vitreous body to release the drug into the eyes gradually over an 8 months period. It may require repeated treatment.
Keratitis
Keratitis is the infection that affects the cornea. Keratitis is the leading cause of visual impairment in adults. About 70000 cases are reported in the United States of America (USA) annually. The disease progression is very fast and can cause a lot of damage before initiating treatment.
 |
| Keratitis Image gallery |
Symptoms
1. Pain in the eye
2. Photophobia
3. Blurred vision
4. Corneal opacity or hypopyon (pus inside)
5. Contact lens wearers experience red eyes or increasing pain
Causes
It can be caused by bacteria, virus or fungi.
Bacteria Keratitis
Bacteria keratitis is more common than other types and can be caused by staphylococcus aureus, coagulase negative staphylococcus, streptococcus pneumoniae and pseudomonas aeruginosa. Among the bacteria keratitis, pseudomonas aeruginosa is more prevalent. Acanthamoeba is experienced by those who swim a lot especially in rivers.
Rural areas experience more fungal keratitis where it presents with trauma and vegetative matter.
Diagnosis
The use of slit lamps and further investigation require corneal scraping sent for gram staining and culture.
Pharmacotherapy/Treatment
Treatment can be initiated with only one approach.
Topical antibiotic
1. Ciprofloxacin 0.3% 1-2 drops every hour for the first 48 hours then every 4 hours
2. Ofloxacin 0.3% 1-2 drops every hour for the first 48 hours then every 4 hours
3. Fortified aminoglycoside (cephalosporin combination)
4. Fortified cefazolin 5% plus gentamicin 0.9% 1-2 drop every hour for 48 hours then reduce according to response.
Fluoroquinolones are better because they reduce the risk of chemical conjunctivitis and ocular discomfort. Ciprofloxacin increases the risk of white corneal precipitation. Chloramphenicol is a bacteriostatic agent and it is unfortunately not active against one of the main causes of bacteria keratitis which is pyrogen aeruginosa. And because the infection can cause a lot of damage in a short time, it is best to avoid chloramphenicol.
Herpes Simplex Keratitis (Ocular Herpes)
It can cause blindness. It affects the cornea, that is the clear front portion of the eye. It is estimated to affect about 1.5 million people worldwide. There are about 20000 new infections yearly. Because of recurrence, about 40000 new cases of severe monocular visual impairment or blindness are reported yearly from herpes simplex keratitis.
It is the most common cause of blindness associated with cornea damage in the USA. It is also the most common cause of infection related blindness in the world. It is estimated that over 90 percent of adults above 50 years of age have been exposed to HSV. HSV 1 infects the cornea, retina, eyelids and conjunctiva. HSV cannot be eradicated from the body. It remains dormant and can reactivate from time to time. Affect men more.
Classification
It is classified based in the layer of the corner that is infected.
1. Epithelial: thin outermost layer of the cornea
2. Stromal: deep layer of the cornea and can be very serious
3. Endothelial
4. Mixed
Epithelial keratitis is more common. There are sometimes you may hear primary or secondary. It is used to distinguish between someone who is having it diagnosed for the first time or a recurring infection.
Symptoms
Stromal herpes simplex virus present with or without ulceration, scarring or vascularisation. Endothelial keratitis is known by keratic precipitates on the endothelium and corneal oedema.
Generally, keratitis presents with pain, inflammation, redness, tearing of the cornea surface, photophobia, blurry vision, mucus discharge, red eye, inflamed eyelids (blepharitis). Affects one eye in most cases.
Cause
HSV is picked up from direct contact with contaminated surface or fluid. Genital herpes is sexually transmitted and is associated with HSV type 2.
Diagnosis
Epithelial herpes simplex virus keratitis manifests as a dendrite ulcer which can be diagnosed by fluorescein staining and a cobalt blue light.
Pharmacotherapy/Treatment
Topical acyclovir ointment applied five times a day for 14 days can clear the infection. Oral acyclovir and valacyclovir can be added to make it faster. Steroids help in relieving itch and pain including inflammation. Brushing the surface of the cornea with a cotton swab after applying numbing drops to remove dead cells.
Epithelial: antiviral ointment and drops e.g acyclovir oral
Stromal: antiviral and steroids drops. Steroids drops can be applied every 2 hours up to 2 weeks while acyclovir can be applied 5 times a day.
Improvement will be noticed within 2-5 days and clear within 2-3 weeks. Recurrent yearly infection may require cornea transplant surgery (keratoplasty).
Infectious Endoptithalmitis
This is an inflammation inside the eye.
 |
| Infectious endoptithalmitis |
Cause
It is caused by bacteria. Most common bacteria is staphylococcus aureus, streptococcus and gram negative bacilli. Infection that occurs in the eye due to eye surgery or eye injury.
Symptoms
Symptoms appear within 1-2 days after exposure to infection but sometimes up to 6 days.
Types Of Endoptithalmitis
Exogenous: it is an infection that goes to the eye through an outside source.
Endogenous: it is when the infection is spread to the eye from other parts of the body.
Exogenous is the more common form especially from cataract surgery. That is because it is the major source of injury to the eyes. Cause of endogenous endophthalmitis are loss of fluid behind the eye, poor wound healing and longer surgery time.
Major symptoms
1. pains in eye
2. Decrease or loss of vision
3. Swollen eyes
4. Red eyes
5. Pus from eyes
Milder symptoms
That occur after 6 weeks from exposure to infection
1. Blurred vision
2. Mild eye pain
3. Photophobia
Risk Factors
1. Cataract
2. Surgery
3. Intravitreal injection
4. Trauma
5. Filtering bleb (for glaucoma)
6. Corneal infection
7. Bacteraemia or fungemia
8. Leaving eye injury untreated
2. Damage to the lens
3. Living in rural areas
4. Glaucoma surgery
Diagnosis
Ultrasound to check for the presence of foreign matters in the eyes. A vitreous tap is used to investigate for infection.
Pharmacotherapy/Treatment
Intravitreal ceftazidime or vancomycin injected by an opthamologist is effective to treat the disease condition. Vitrectomy may be beneficial to avoid loss of vision. Oral ciprofloxacin 750mg (20mg/kg up to 750mg) plus intravenous (IV) vancomycin (adult and child 15mg/kg) is another alternative. Also, gentamicin (adult and child 5mg/kg) IV plus cefazolin 2g (child 50mg/kg up to 2g) can be given.
Vancomycin and aminoglycoside or a third generation cephalosporin given orally. IV clindamycin, gentamicin, ceftriaxone and cefotaxime are also effective. IV vancomycin 1mg/0.1ml is used for gram positive bacteria. Amikacin 0.4ug/0.1ml and ceftazidime which is suitable for gram negative bacteria is also recommended but care should be taken because of its retina toxicity and lipopolysaccharide induced inflammation. Intravitreal amphotericin B 5-10ug/0.1ml and oral fluconazole is used for fungi infection.
Stye
Stye is a pimple or abscess that forms on the upper or lower eyelid. It is called hordeolum. It usually begins like a pimple next to an eyelash. It eventually becomes red, painful which bursts and heals after some days. It can appear on the eyelids which are external or inside the eyelids which are internal. External stye appears with a whitehead which is not the case with internal stye.
Chalazion is a type of stye that forms a scar without pain. It does not affect eyesight. It happens at any age and tends to reappear from time to time especially in people with blepharitis or rosaceae (skin).
 |
| Stye Image gallery |
Symptoms
It is simply described as feeling a red hot swollen tender bump near the edge of the eyelid. A chalazion appears as a tender, smooth, round bump in the middle of the eyelid.
Cause
Bacteria block the oil duct. When the oil can no longer flow, the area becomes inflamed. It can also be formed when germs and dead skin cells get trapped at the edge of the eyelid.
Pharmacotherapy/Treatment
It is self limiting that lasts between 7-10 days but there are home management tips. A warm compress for like 10-15 minutes 2-4 times a day up to several days can help. Applying pressure in the inflamed bump also helps to unplug the oil gland. The bump must never be squeezed or pinch but allowed to rupture on its own.
Stye that spreads to the skin or recurrent stye needs oral and topical antibiotic management. Antiinflammatory drugs help with the inflammation but when none of these are effective, surgery is carried out.
Paracetamol and ibuprofen are best choice pain medication. The choice of antibiotics is determined by the type of bacteria causing it.
Oral
Cephalexin 500mg every 12 hours for 7 days is recommended. Amoxicillin and clavulanic acid given two times a day for 7 days is another alternative. Also, azithromycin 500mg on day one and 250mh for another 4 days can be used. Lastly, levofloxacin 500mg daily for 7 days and ciprofloxacin 500mg every 12 hours for 7 days is effective.
Topical
Azithromycin eye drop
Orbital Cellulitis
Eye cellulitis or periorbital cellulitis is an infection of the soft tissue and fat that hold the eyes in its socket. It is not contagious and can affect anyone. However, it is more in children below 9 years than adults. The condition is painful and uncomfortable. It can be dangerous when not treated. It can be life threatening which can lead to blindness.
 |
| Orbital cellulitis |
Cause
It is caused mostly by streptococcus species and staphylococcus aureus. Other bacteria and even fungals are responsible too. Orbital cellulitis in children below 9 is usually caused by one type of bacteria. Up to 98 percent of orbital cellulitis start out as untreated bacterial sinus infection which spreads behind the orbital septum. The orbital septum is a thin, fibrous membrane that covers the front of the eye. Wounds, bug bites and animal bites near the eyes are a source of infection but can be gotten from infection that spreads from other parts of the body.
Symptoms
1. Protruding eye (proptosis)
2. Pain in or around the eye
3. Nasal tenderness
4. Swelling of the eye area
5. Inflammation and redness
6. Inability to open the eyes
7. Pain moving the eyes
8. Vision loss
9. Discharge from eyes or nose
10. Fever and headache
Diagnosis
1. CT scan or MRI imaging of head, eye and nose
2. Examination of the nose, teeth and mouth
3. Blood eye discharge or nasal culture
Pharmacotherapy/Treatment
Admission into the hospital is required to commence treatment. Vancomycin, ampicillin/sulbactam 50m/kg IV every 6 hours for children or 1.5-3g IV every 6 hours for 7 days is given for inpatients. A second or third generation cephalosporin such as cefotaxime 50mg/kg IV every 6 hours in children or 1-2g IV every 6 hours in adults for a period of 14 days optional when sinusitis is present. Imipenem, ceftriaxone and piperacillin/tazobactam are other viable options.
If cellulitis is related to trauma or presence of foreign body, vancomycin 1g in every 12 hours or ertapenem 100mg IV daily for 7-10 days is recommended. Outpatients can be given oral clindamycin, septrim or doxycycline, amoxicillin and clavulanic acid.
Surgery may be required which is done to decompress the orbital and drain the abscess and open up the infected sinuses.
Blepharitis
Inflammation around the base of the eyelash that affects the eyelids causing clumping and stickiness around the eyelash. It can affect anyone at any age and time. The chronic form is more common than the acute form.
 |
| Blepharitis |
Cause
There are many causes. They are inflammatory reactions to bacteria that normally live in eyelids.
1. Seborrhoeic dermatitis or rosacea
2. Parasite: demodex eyelash mites
3. Herpes simplex virus
Risk Factors
1. Dandruff
2. Dysfunctional of meibomian glands on the rims of the eyelids. These oily substance prevent the eyes film of tears from evaporating
Symptoms
Redness and stickiness of the eyelid with clumping of scaly skin around the base of the eyelash. Itchy eyelids, irritated and watery eyes with flaking and crusting at the base of the eyelash similar to dandruff burning. Others are stinging eyes, photophobia, gritty feeling in the eyes and the sensation of having something in the eye.
Symptoms are more pronounced in the morning. It can affect both eyes at the same time but it is not a sight threatening problem with decreased vision. Symptoms can be in waves like a pause that flare-up. Some conditions are comorbidity like ocular rosacea, psoriasis and seborrheic dermatitis.
Types
Anterior: this affect the front edge where the eyelash join
Posterior: this affects the inner edge of the eyelid where it meet the eyeball.
Diagnosis
Slit lamp examination
Pharmacotherapy/Treatment
There is no cure for blepharitis. Steroids drops or oral steroids is for pain, itchy and inflammation of the eye. Oral, drops and ointment antibiotic is to fight the infection. Artificial tears drop is for those with itchy eyes from dry eyes. Best artificial tears drop should be without preservatives. The use of warm compresses is meant to loosen the crust. Massaging the eyes is to loosen the small oil glands while eyelid cleaning removes crust.
Uveitis
Uveitis is an eye condition whereby the middle layer of the eye (pars plana and iris), the uvea (choroid) and surrounding tissues (ciliary body) get inflamed. It leads to vision loss and it can affect one or both eyes. Most common is iritis. Common to hear uveitis also referred to as uveal layer, uveal cord, uveal tract and vascular tunic.
 |
| Uveitis Image gallery |
Symptoms
Symptoms may appear gradually or suddenly.
1. Pain
2. Red eyes
3. Cloudy vision or blurry vision
4. Spots in the eyes that look like tiny rods of chain of transparent bubbles floating around in the field of the vision.
5. Photophobia
6. Headache
7. Small pupil alterations of colour if the iris
Cause
An injury to the eyes, bacteria, virus and or underlying disease condition. It affects people between the age of 20 and 60 years of age. Human immunodeficiency virus/Acquired immune deficiency syndrome (HIV/AIDS), brucellosis, herpes simplex virus, herpes zoster virus, leptospirosis, lyme disease, syphilis, toxocariasis, toxoplasmosis and tuberculosis are the underlying health condition that can lead to uveitis.
Types
Anterior: this is also known as iritis. This is the inflammation of the iris. Iridocylitis is similar but that affects the ciliary body.
Intermediate: can be either vitrilitis or pars planitis (jelly like part of the eye).
Posterior: inflammation of the retina and choroid later (back of the eye). This is the least common but more serious.
Pen-uveitis: this is the inflammation of all layers of the uvea.
Read Also: Sniper insecticide can kill when applied to the head to treat lice
Diagnosis
Slit lamp, blood test and x-ray
Complications
1. Glaucoma
2. Cataract
3. Macular
4. Odema
5. Scar tissue
6. Retina detachment or detached retina
7. Vision loss
Pharmacotherapy/Treatment
First is to find out the cause of the uveitis. If there is an underlying condition, it should be treated. The following should help for anterior;
1. Glasses
2. Eye drops to dilate the pupil and reduce pain
3. Steroid eyedrops to reduce irritation and inflammation
For posterior;
Oral steroid, injection around the eyes and antibiotics.
For intermediate;
1. Steroid eye drop and oral
2. The immune system can be suppressed if it is the underlying cause. Immune suppressors include azathioprine, cyclosporine, methotrexate and mycophenolate. Biologics such as abatacept, adalimumab, daclizumab infliximab, rituximab are the recent drugs of choice.
Vitrectomy surgery drains the liquid and implants for posterior uveitis contain steroid (fluocinolone) to treat inflammation for 2-3 years. Oral ibuprofen can be added.
Posterior heals slowly and anterior goes away within a few days with treatment. Posterior is dangerous if it lasts for months due to the presence of other conditions such as permanent vision loss.

Hi, I visited your website and I really like your website, you have got great information. I have a site for you please to share
ReplyDelete