Pharmacotherapy/Treatment Of Gastroesophageal Reflux Disease (GERD)
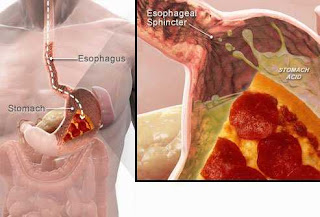
Gastroesophageal reflux disease (GERD) is when stomach acid flows back into the esophagus. The acid can be liquid or gas. It can be minor when it happens a few minutes in a week or major when it happens for hours everyday. It affects people of all ages including newborns.
 |
| Gastroesophageal reflux disease (GERD) |
Symptoms Of GERD
Symptoms can be severe and can include one or more. It can last for two hours. Symptoms can get worse mostly after eating, lying down, bending over or at night. At night, saliva production reduces which is one of the ways the acid in the stomach is neutralised naturally. This leads to reduced swallowing. Also, little or no gravitational effect during sleep makes GERD symptoms worse.
Read Also: How To Manage Baby Acid Reflux
1. Heartburn usually after eating
2. Chest pain that looks like heart failure
3. Difficulty swallowing
4. Regurgitation of food or sour liquid
5. Bad breath especially in children
6. Wearing away of the tooth enamel
7. Sensation of lump in the throat
8. Nighttime acid reflux that result in cough
9. Laryngitis
10. New or worsening asthma
11. Strictures which is the narrowing of the lumen due to scar formation
Complication Of GERD
1. Esophageal ulcer
2. Esophageal stricture
Cause Of GERD
It is cause by weakening or relaxation of the lower esophageal sphincter (LES)
Risk Of GERD
1. Obesity
2. Hiatal hernia
3. Pregnancy
4. Delay stomach emptying
5. Connective tissue disorder
6. Smoking
7. Eating large and heavy meals (fatty and fried food)
8. Eating late at night
9. Coffee and alcohol
10. Aspirin
11. Rheumatoid arthritis (RA)
12. Gastroparesis
Pathophysiology Of GERD
The pathogenesis of gastro-oesophageal reflux disease is multifactorial, involving transient lower esophageal sphincter relaxations and other lower esophageal sphincter pressure abnormalities. As a result, reflux of acid, bile, pepsin and pancreatic enzymes occurs, leading to esophageal mucosal injury. Other factors contributing to the pathophysiology of gastro-oesophageal reflux disease include hiatal hernia, impaired esophageal clearance, delayed gastric emptying and impaired mucosal defensive factors. Hiatal hernia contributes to gastro-oesophageal reflux disease by promoting lower esophageal sphincter dysfunction. Impaired esophageal clearance is responsible for prolonged acid exposure of the mucosa. Delayed gastric emptying, resulting in gastric distension, can significantly increase the rate of transient lower esophageal sphincter relaxations, contributing to postprandial gastro-oesophageal reflux disease. The mucosal defensive factors play an important role against development of gastro-oesophageal reflux disease, by neutralizing the back diffusion of hydrogen ions into the oesophageal tissue. While the pathogenesis of esophageal symptoms is now well known, the mechanisms underlying extra-esophageal airway manifestations are still poorly understood. Two hypotheses have been proposed: direct contact of gastric acid with the upper airway and a vago-vagal reflex elicited by acidification of the distal oesophagus, leading to bronchospasm. In conclusion, gastro-oesophageal reflux disease can be considered as the result of a complex interplay of factors, all promoting the contact of gastric acidic contents with the esophageal mucosa, leading to different degrees of esophageal damage.
Read Also: When To Take Antisecretory Drugs And Antacids In Relation To Food
Complication Of GERD
1. Narrow esophagus due to scar formation from acid burning the esophagus
2. Open sore in the esophagus
3. Vomiting
4. Precancerous changes
Diagnosis Of GERD
1. Physical examination including interview
2. Upper endoscopy which is the observation of the esophagus
3. Biopsy
4. Ambulatory acid probe test: this is the use of a computer to collect the pH of the esophagus. A small tube is inserted into the esophagus to collect the pH reading and is connected to a monitor that keeps giving out the result. The result gives a daily report of how frequent acid enters the esophagus.
5. Esophageal manometry: this device is connected to the LES to monitor the rythmsm muscle of contraction after swallowing. It also measures the coordination and force exerted by the muscles.
6. X-ray is taken after drinking a chalky liquid that coats and fills the inside lining of the digestive tract. The coating allows your doctor to see a silhouette of your esophagus, stomach and upper intestine. You may also be asked to swallow a barium pill that can help diagnose a narrowing of the esophagus that may interfere with swallowing.
Pharmacotherapy/Treatment Of Gastroesophageal Reflux Disease (GERD)
Antacids
Antacid neutralises acid in the esophagus and stomach. They are given when symptoms occur. There are many types of antacids and come in different forms. Antacids may be aluminum, magnesium, or calcium based. They can be formulated into tablets which must be chewed with water to be effective or liquid. Calcium-based antacids (usually calcium carbonate), unlike other antacids, stimulate the release of gastrin from the stomach and duodenum. Gastrin is the hormone that is primarily responsible for the stimulation of acid secretion by the stomach. Therefore, the secretion of acid rebounds after the direct acid-neutralizing effect of the calcium carbonate is exhausted. The rebound is due to the release of gastrin, which results in an overproduction of acid. Theoretically at least, this increased acid is not good for GERD.
Some antacids come with simethicone, a compound that reduces stomach gas. Gas helps push liquid and gas acid into the esophagus against gravity as hot gas is known to rise. Also, some come with alginate, a compound that forms a barrier around the acid in the stomach preventing the acid to reflux into the esophagus. It also coats the injured sore in the esophagus and stomach.
Magnesium can cause diarrhea. Using an antacid that contains only aluminum along with this product can help control diarrhea. The aluminum in this product can cause constipation. To minimize constipation, drink plenty of fluids and exercise. Diarrhea is more common with this product than constipation.
Aluminum-containing antacids bind to phosphate, an important body chemical, in the gut. This can cause low phosphate levels, especially if you use this medication in large doses and for a long time.
Also, antacid agents require caution in patients with:
1. Renal failure
2. Heart failure
3. Edema
4. Cirrhosis
5. Low-sodium diets
6. Uremia
7. GI hemorrhages
8. Hyperparathyroidism
9. Renal calculus
10. Achlorhydria
Generally, the dose is dependent on the severity. The average therapeutic dose of antacid is 10 to 15 mL (1 tablespoon or one package content) of liquid or 1 to 2 tablets 3 to 4 times a day. Calcium Carbonate is used up to a maximum dose of 8000 mg per day up to 2 weeks with 1 to 4 tablets for symptomatic relief. Aluminum Hydroxide is usually taken daily after meals and at bedtime at a dose of 640 mg up to 5 to 6 times a day with a maximum dose of 3840 mg per 24 hours. The dose for suspension form is 320 mg/5 mL (473 mL). The suspension is to be shaken before use and is to be followed by water.
Antacids containing aluminum salts are safe to be used in pregnant women as well as for women during labor for aspiration prophylaxis. The information regarding the use of aluminum-containing antacids in breastfeeding females has not been studied, but aluminum is known to be endogenous to breast milk. In the case of calcium-containing antacids, excessive use is to be avoided in pregnant women as calcium crosses the placenta. The amount of calcium reaching the fetus is dependent on the physiological changes in the mother. Maternal calcium intake also affects the amount of calcium excreted in breast milk; the currently prevailing opinion is that the use of calcium-containing antacids is safe during breastfeeding.
Antisecretory Ulcer Drugs
The histamine 2 receptor blockers (H2) and proton pump inhibitors (PPI) lower the amount of acids released in the stomach. The H2 blockers can heal the oesophagus but not as much as how the PPI does. PPI are better in treating the symptoms than H2 blockers. Side effects of PPIs include headache, diarrhoea and stomach upset. There is a link with using PPI and clostridium difficile infection. It could be due to the acid lowering effect reducing the amount of acid available in the stomach that kills bacteria that come with food.
The advantage of a PPI over an H2 antagonist is that the PPI shuts off acid production more completely and for a longer period of time. Not only is the PPI good for treating the symptom of heartburn, but it also is good for protecting the esophagus from acid so that esophageal inflammation can heal.
Pro-kinetic drugs (promotility) are drugs that stimulate the muscles of the gastrointestinal tract. This includes the esophagus. They increase stomach emptying time thereby preventing the possibility of stomach acid coming up. Examples are metoclopramide and domperidone. Another mechanism of action attributed to these drugs is that it increases the pressure in the muscles and strengthens the contraction (persistasis) of the esophagus. They are added to some ulcer drugs.
Read Also: Pharmacotherapy/Treatment Of Peptic Ulcer
Another drug that works in GERD is baclofen. It decreases the frequency of relaxation of the sphincter. Side effects include fatigue or nausea.
Surgery
There are several surgeries available for treating GERD. They are;
1. Fundoplication: this is the sewing of the top of the stomach around the LES. This helps to add pressure.
2. Geriatric surgery: is done to remove fat from the body to reduce weight.
3. Endoscopy: is delivery of radio frequency energy to the sphincter. It is not always used.
4. LINX device: here a ring with a tiny magnetic head is placed in the LES. The attraction closes the esophagus to acid reflux but weak enough to allow food pass.
5. Transoral incisionless fundoplication (TIF): In this surgery, the LES is tightened by creating a partial wrap around the LES using polypropylene fasteners.
Lifestyle Modification
1. Reduce weight
2. Raise head during sleep
3. Quit smoking
4. Eat small food
5. Do not lie immediately after a meal. Wait for like 30 minutes
6. Avoid tight fitting clothing

Comments
Post a Comment
Please have your say