Pharmacotherapy/Treatment Of Tuberculosis
Tuberculosis (TB) is an infectious contagious disease. This disease affects mostly the lungs. When it affects the lungs, it is called pulmonary TB. It can also spread to other parts of the body like the brain and spine. When it affects other parts of the body, it is called extrapulmonary TB.
Extrapulmonary tuberculosis is TB within a location in the body other than the lungs. This occurs in 15–20% of active cases, causing other kinds of TB. These are collectively denoted as "extrapulmonary tuberculosis". Extrapulmonary TB occurs more commonly in immunosuppressed persons and young children.
Other organs that can be affected include the lining covering the lungs (pleural TB); the central nervous system (TB meningitis); bone and joints (musculoskeletal system); lymph nodes; abdomen – where the liver, spleen and the intestines can be affected (abdominal TB); kidney and bladder (urogenital TB); and blood.
Read Also: Treatment of pneumonia
A study conducted in Johannesburg showed that the most common sites of extra pulmonary TB were the pleura (39.1%), lymph nodes (31.0%), blood (21.8%), central nervous system (7.3%), and abdomen (2.9%).
Ocular TB is defined as an infection by TB in the eye, around the eye, or on its surface. Ocular TB is usually not associated with clinical evidence of pulmonary TB, as up to 60% of extrapulmonary TB patients may not have pulmonary TB.
Without treatment, about 45 percent of TB patients with HIV will die. There are more cases in developing countries. Undernourished are three times more at risk. There are 2.3 million new infection cases in 2018 attributed to malnutrition. Alcohol and tobacco smoking increase TB disease by a factor of 3.3 and 1.6 respectively. In 2018, 0.83 million new TB were attributed to alcohol use disorder and 0.86 million attributed to smoking. 1.1 million children between the age of 0-14 years contracted TB and 230000 children died in 2018.
Cases in the South East Asia region are 45 percent, Africa is 24 percent, west Pacific is 18 percent in 2018. There are about 87 percent of cases in just 30 countries. Eight countries accounted for two third of new infection (India, China, Indonesia, Philippines, Pakistan, Nigeria, Bangladesh and south Africa)
Cause Of Tuberculosis
It is caused by a bacteria known as mycobacterium tuberculosis (MTB). Others of less severe nature are mycobacterium bovis, mycobacteria africanism, mycobacterium canettii and mycobacterium microti.
Stage Of Tuberculosis
Latent TB (LTB): this happens when the person is positive to TB from laboratory investigations without clinical signs and symptoms. It happens when the person's immune system is strong enough to fight back on the bacteria but not strong enough to clear it off the system. The person remains asymptomatic and not contagious for many years.
About one third of the world population have latent TB. About 5-15 percent will eventually enter the active stage. This happen due to weakened immune system by things like HIV, malnutrition, diabetes, kidney disease, head and neck cancer treatment such as chemotherapy, low body weight, medication for organ transplant, certain drugs to treat rheumatoid arthritis, chrohn disease, psoriasis, tobacco smoking, alcohol and lastly children.
Miliary TB: is a rare form of active disease that occurs when TB bacteria find their way into the bloodstream. In this form, the bacteria quickly spread all over the body in tiny nodules and affect multiple organs at once. This form of TB can be rapidly fatal.
Active TB: active TB comes with full symptoms of any part of the body. It can be from a recent exposure to the bacteria or breakdown of immune defence of latent TB. Most latent TB will develop to be active when the immune system is broken down due to infection or other factors that can weaken the immune system.
People with active TB infect about 5-15 percent of people around them in a space of one year if they don't start treatment on time. It takes about 2-3 weeks after starting treatment that they are no longer contagious.
Types Of Drug Resistant TB
Multi drug resistant tuberculosis (MDR TB): this is defined as the resistance of tuberculosis bacteria to the two most potent drugs available which are isoniazid and rifampicin. There are about 484000 new cases of rifampin resistance TB in 2018. 78 percent had MDR TB. Russia, China and India had more burden making half of all cases. About 6.2 percent of MDR TB had XDR TB.
Extensive drug resistant tuberculosis (XDR TB): This is a situation whereby the tuberculosis bacteria is resistant to isoniazid, rifampicin, any of the second line drugs (fluoroquinolone) and at least one of the three second line injection (amikan, kanamycin and capreomycin).
Symptoms Of Tuberculosis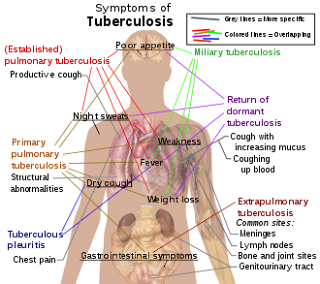
Tuberculosis
Image: wiki
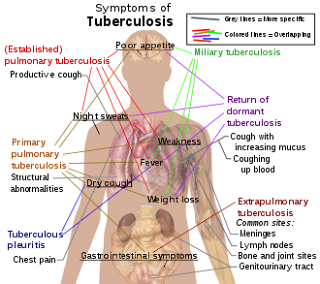
Image: wiki
1. Cough with sputum for more than three weeks
2. Chest pain
3. Cough with blood
4. Feeling tired at all times
5. Nith sweat
6. Chills
7. Fever
8. Loss of appetite
9. Weight loss
The cough, fever, night sweat and weight loss appear mild for several months making it hard for patients to seek medical attention.
Symptoms of tuberculous meningitis may include the following:
1. Headache that has been either intermittent or persistent for 2-3 weeks
2. Subtle mental status changes that may progress to coma over a period of days to weeks
3. Low-grade or absent fever
Symptoms of skeletal TB may include the following:
1. Back pain or stiffness
2. Lower-extremity paralysis, in as many as half of patients with undiagnosed Pott disease
3. Tuberculous arthritis, usually involving only 1 joint (most often the hip or knee, followed by the ankle, elbow, wrist, and shoulder)
Symptoms of genitourinary TB may include the following:
1. Flank pain
2. Dysuria
3. Frequent urination
3. In men, a painful scrotal mass, prostatitis, orchitis, or epididymitis
4. In women, symptoms mimicking pelvic inflammatory disease
Symptoms of gastrointestinal TB are referable to the infected site and may include the following:
1. Nonhealing ulcers of the mouth or anus
2. Difficulty swallowing (with esophageal disease)
3. Abdominal pain mimicking peptic ulcer disease (with gastric or duodenal infection)
4. Malabsorption (with infection of the small intestine)
5. Pain, diarrhea, or hematochezia (with infection of the colon)
Signs of extrapulmonary TB differ according to the tissues involved and may include the following:
1. Confusion
2. Coma
3. Neurologic deficit
4. Chorioretinitis
5. Lymphadenopathy
6. Cutaneous lesions
Complications
1. Joint damage
2. Lung damage
3. Infections or damage to the bones, spinal cord or lymph nodes
4. Liver or kidney problem
5. Inflammation of the tissues around the heart
6. Low birth weight
Mode Of Transmission
It is contagious but not like cases of covid-19. Most infections happen between family members or very close friends. The bottom line is spending long times together.
The bacteria is present in saliva. It does not live on surfaces and skin. It is contracted when contaminated droplets are inhaled or breathed in. However, some research currently claims that some cases of the bacteria passing through the skin have been recorded.
1. Coughing
2. Sneezing
3. Talking
4. Laugh
5. Spit
There are about 3000 bacteria in a single cough. 10 bacteria is enough to cause infection. Replication of mycobacterium is not as fast as other bacteria as it can take up to two days. In two to three weeks, between 1000 to 10000 copies have been made. This can be detected by tuberculin skin test.
Risk
1. Number of bacteria expelled
2. Concentration of bacteria
3. Length of exposure
4. Immune response
Diagnosis
Diagnosis of TB is not very straight forward. Direct tests for the bacteria can come out false positive or false negative. The reason is that some of the tests are always positive for those who got vaccines at early childhood and negative for newly infected individuals.
Some other tests check for biological markers. This is just a guide if the person may likely be infected with the bacteria.
1. Skin test/Mantoux tuberculin skin test: the process involves injecting a liquid into the skin of the lower arm. Swelling of 5mm or more after 2-3 days is recorded as positive to TB. False positive and negative is common.
2. Interferon gamma release assay (IGRAs)/Blood test: measure response rate when TB proteins are mixed with a small amount of blood.
Others are: Acid-fast bacillus (AFB) which is the gold standard in laboratory, Specific enzyme-linked immunospot (ELISpot), Nucleic acid amplification tests and Blood culture. Computer tomography (CT) scan and chest x-ray to look for changes in lungs which help to determine if it is in latent phase or active phase.
Positive cultures should be followed by drug susceptibility testing; symptoms and radiographic findings do not differentiate multidrug-resistant TB (MDR-TB) from fully susceptible TB. Such testing may include the following:
1. Direct DNA sequencing analysis
2. Automated molecular testing
3. Microscopic-observation drug susceptibility (MODS) and thin-layer agar (TLA) assays
4. Additional rapid tests (eg, BACTEC-460, ligase chain reaction, luciferase reporter assays and FASTPlaque TB-RIF).
Patients that are positive should also be screened for human immunodeficiency virus (HIV) serology. Most HIV patients always come down with TB.
Rapid test xpert MTB/RIF is approved by the world health organisation because it can detect TB and resistance to one of the most effective agents against the drug, rifampicin with result ready within 24 hours.
Pharmacotherapy/Treatment Of Tuberculosis
The treatment depends on the type of TB and the stage. Treatment for a short time using multiple therapy has greater advantage than the use of a single drug for a long time. Treatment can last for a minimum of 6 months even up to 2 years. Early months require the use of many drugs that are scaled down to just some few after several months of treatment when positive response is recorded.
There is growing concern about the resistance of tuberculosis bacteria to available drugs. Resistance is growing due to incorrect prescription, the use of low quality drugs, and patient failure to adhere to treatment guidelines due to long duration of treatment.
Latent TB (LTB)
Latent TB is usually treated with one or two drugs for as short a time as possible. It can be for 6 months. Treatment for 9 months is also possible if the person was exposed to a TB patient that has MDR TB or XDR TB. Treatment is initiated for those with positive TB blood tests. Those with IGRAs of 5 mm or more with other risky situations like HIV should start treatment.
As of 2018, there are four CDC-recommended treatment regimens for latent TB infection that use isoniazid (INH), rifapentine (RPT), and/or rifampin (RIF). All the regimens are effective and should be used for nine months.
The recommended 2020 LTBI treatment guidelines include three preferred rifamycin-based regimens and two alternative daily-isoniazid monotherapy regimens. These recommendations are intended for Mycobacterium tuberculosis infections with presumed susceptibility to isoniazid or rifampin. M tuberculosis strains that are resistant to both isoniazid and rifampin are exempt from these recommendations.
Generally, rifamycin-based treatment regimens administered in short courses are preferred over isoniazid monotherapy administered in longer courses for the treatment of LTBI.
1. Once-weekly isoniazid plus rifapentine for 3 months (strongly recommended in adults and children >2 years, including those with HIV infection) OR
2. Daily rifampin for 4 months (strongly recommended in HIV-negative adults and children of all ages) OR
3. Daily isoniazid plus rifampin for 3 months (conditionally recommended in adults and children of all ages and in HIV-positive persons).
Alternative treatment regimens for LTBI
1. Daily isoniazid for 6 months (strongly recommended in HIV-negative adults and children of all ages and conditionally in HIV-positive adults and children of all ages) OR
2. Daily isoniazid for 9 months (conditionally recommended in adults and children of all ages regardless of HIV infection status)
Active TB
The treatment for active TB requires at least four drug combinations for four months. Another combination of two drugs for another two months. TB test is carried out every month to confirm if the drug is working. In case the drug does not elicit the right response, alternative therapy is initiated. Cure rate of 95-97 percent.
Read Also: Treatment of STI
Active TB is treated with first line therapy. First line therapy is a drug that is effective and safe. They are ethambutol, isoniazid, pyrazinamide and rifampin. Treatment can span up to 12 months. Ethambutol can be changed to streptomycin. Some of the combination are;
1. Isoniazid (INH), rifampin, pyrazinamide, ethambutol
a. Once daily for 8 weeks (56 doses)
or five times per week for 8 weeks (40 doses)
b. Once daily for 2 weeks, then twice weekly for 6 weeks (26 doses) or five times per week for 2 weeks, then twice weekly for 6 weeks (22 doses)
c. Three times per week for 8 weeks (24 doses)
2. Isoniazid, rifampin, ethambutol
Once daily for 8 weeks (56 doses)
or five times per week for 8 weeks (40 doses).
Relapse is possible in 0.4 percent within 2 years
MDR TB
Treatment includes a combination of second line therapy. They are fluoroquinolone, injectable antibiotics (amikacin, capreomycin and kanamycin), ethionamide, para-amino salicylic acid, pretomanid, bedaquiline and linezolid. Duration of treatment depends on so many factors. Treatment can be for as long as two years. This can be expensive and toxic. Cure rate of MDR TB is 50-60 percent.
The intensive phase of MDR-TB treatment should consist of at least four second-line anti-TB drugs that are likely to be effective (including an injectable anti-TB drug), as well as pyrazinamide. MDR regimens should include at least pyrazinamide, a fluoroquinolone, an injectable anti-TB drug, ethionamide (or prothionamide) and either cycloserine or para-amino salicylic acid. MDR-TB treatment regimen consisting of combinations of later-generation fluoroquinolones (moxifloxacin or gatifloxacin), clofazimine, ethambutol and pyrazinamide throughout the treatment period supplemented by prothionamide, kanamycin, and high-dose isoniazid during an intensive phase.
XDR TB
This condition is rare. There is not much information about treatment patterns. The world health organisation (WHO) is working with so many research groups to come to a concluding guide for treating XDR TB. Treatment of XDR TB requires a combination of five drugs for treatment and four for maintenance therapy. They include some second line drugs with pretomanid and anitroimidazoxazine. Short regimens last between nine to 12 months when there is no resistance. Presence of resistance will push treatment into two years. Bedaquiline or delamanid may be added. Cure rate is 30-50 percent.
Special populations
Pregnant women must continue to receive treatment to prevent mother to child transmission. Avoid streptomycin in pregnant women. Give pyrazinamide instead. Risk of mother to child transmission during breastfeeding is high. To continue breastfeeding, give pyridoxine to the baby. Isoniazid and rifampicin for six months can be given to children along with pyrazinamide for the first 2 months. Ethambutol should be avoided in children except in resistant cases. This is because it is difficult to monitor visual acuity and color perception Avoid rifampicin in HIV patients on protease inhibitors. Rifabutin should be used instead. Tuberculosis meningitis responds well to dexamethasone with regular anti-TB drugs..
Adult Doses
Isoniazid 300mg daily
Rifampicin 600mg daily
Rifapentine 750-900mg with isoniazid 900mg once a week for 12 months
Surgery
When treatment seems not to work, surgical resection of the lungs is used. It helps to reduce the burden of the bacteria in the lungs. This further enhances therapy as the drugs have less bacteria to fight. They are segmentectomy, contectomy, pneumonectomy and pleurectomy
Prevention
1. The use of facemask by infected persons or close relatives
2. Bacille Calmette-Guérin vaccine. It is not used in the United States of America (USA). it is not 100 percent effective and does not last more than three months. Suitable for children in endemic areas. It is given for three months.
3. Isoniazid preventive therapy
List Of Drugs Use In TB
1. Isoniazid Tablets (50, 100, and 300 mg), elixir (50 mg per 5 mL), aqueous solution for IV or IM injection (100 mg per mL)
2. Rifampin Capsules (150 and 300 mg; powder may be suspended for oral administration), aqueous solution for IV injection
3. Pyrazinamide Tablets (500 mg, scored)
4. Ethambutol Tablets (100 and 400 mg)
5. Streptomycin
6. Levofloxacin
7. Moxifloxacin
8. Rifapentine Tablets (150 mg, film-coated)
9. Ethionamide
10. Amikacin
11. Cycloserine
12. Capreomycin
13. Rifabutin Capsules (150 mg)
14. Clofazimine
15. Para-aminosalicylic acid
16. Bedaquiline
17. Pretomanid
18. Delamanid
19. Rifampicin

Comments
Post a Comment
Please have your say