Pharmacotherapy/Treatment Of Chronic Obstructive Pulmonary Disease (COPD)
 |
| COPD |
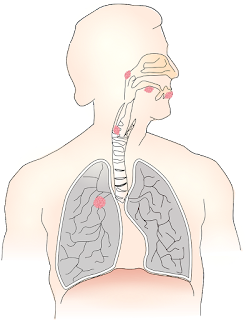
Chronic obstructive pulmonary disease (COPD) is a disease of the lung. It is characterized by persistent reduction in air flow in the lungs. It can get serious and life-threatening if not properly managed. It affects more than 16 million people worldwide. COPD is the fourth leading cause of death worldwide and is expected to be the third leading cause by 2030. It is a progressive disease that affects people above 40 years of age.
Function Of Lungs
When a person with healthy lungs inhales air, it travels down their windpipe and into the airways of the lungs, known as bronchial tubes.
Inside the lungs, the bronchial tubes branch into thousands of smaller, thinner channels called bronchioles.
At the end of these tubes are bunches of tiny round air sacs called alveoli. There are more than 300 million alveoli in the lungs. Larger lungs have more alveoli.
Read Also: Treatment of asthma
Capillaries are small blood vessels that surround the walls of the air sacs. Once air makes its way to the air sacs, oxygen passes through the walls of the air sac into the capillaries that transport blood.
At the same time, carbon dioxide moves from the capillaries into the air sacs. These events happen at the same time, and scientists refer to this as gas exchange.
Healthy air sacs are elastic and very stretchy. As a person breathes in, the air sacs fill up with air like a balloon. As they breathe out, the air sacs deflate due to the air moving out. The body uses energy to blow the air sacs up but does not use any energy to empty them as they return to their original size.
The diseases that makeup COPD include emphysema, chronic bronchitis, and chronic obstructive refractory asthma. Each of these has different effects on the lungs and respiratory system.
Chronic Bronchitis
Chronic bronchitis results from an increase in swelling and mucus production in the breathing tubes or airways. This results in the lining of the airways being constantly irritated and inflamed. The extra swelling and mucus make the inside of the breathing tubes smaller than usual, making breathing more difficult.
Emphysema
Emphysema causes damage to the air sacs in the lungs and the walls between them. This causes the sacs to lose their stretchiness and trap air instead.
It becomes increasingly difficult to expel all air from the lungs, and they no longer empty efficiently. This leads to the presence of more air than usual. This phenomenon is called air trapping and causes the lungs to hyperinflate.
When there is extra air in the lungs, breathing takes additional effort, which contributes to shortness of breath.The damage can also destroy the walls of the air sacs, resulting in larger, less efficient air sacs instead of the smaller ones. This reduces gas exchange within the lungs.
There are three types of emphysema; centriacinar, panacinar, paraseptal. Centriacinar emphysema affects the alveoli and airways in the central acinus, destroying the alveoli in the walls of the respiratory bronchioles and alveolar ducts. Panacinar emphysema affects the whole acinus. Paraseptal emphysema is believed to be the basic lesion of pulmonary bullous disease.
Refractory Asthma
This is a severe type of asthma that does not resolve in response to asthma medications.
Asthma presents in attacks of symptoms that cause the airways to become tighter and more swollen. People with refractory asthma cannot return the airways to their natural state using medications.
GOLD Classification
Global Initiative for Chronic Obstructive Lung Disease (GOLD), an association gave some classification of COPD as grade one to four. They use spirometry test results of force extraction volume 1 (FEV1). This is the amount of air you can breathe out of the lungs in the first seconds of a force extraction. Severity increases as FEV1 decreases.
Grade one: mild
Grade two: moderate
Grade three: severe
Grade four: very severe
Symptoms
1. Breathlessness (need for air)
2. Clear throat especially in the morning
3. Depression
4. High blood pressure in lung arteries
5. Frequent respiratory infections
6. Blue lips of fingernails
7. Chronic cough and spotting that appear white play yellow or greenish
8. Daily light work becomes difficult
9. Wheezing
10. chest tightness
11. Swelling in ankles feet or legs
12. Weight loss
Cause
1. Smoke including secondhand smoke
2. Solid fuel from burning charcoal
3. Asthma
4. Low level of alpha-1-antitrypsin (AAt) is suspected to be one of the causes because in about 1% of COPD patients, AAt is low. AAt is made in the lower and secreted into the bloodstream to help protect the lungs. Deficiency can be due to be genetic factors and can cause liver or lung disease or both.
Risk Factors
1. Smoke especially men as they smoke more. Although recently the tide is tilting as more women embrace smoke
2. Air pollution (solid fuel)
3. Respiratory infections during childhood
Complications
Can cause heart disease and asthma and suspected to cause lung cancer
Diagnosis
1. Spirometry is an instrument that measures the force of exhalation of air from the airway called the breathing test.
2. Lung volume and diffusing capacity
3. Six minutes walk test
4. Pulse oximeter
5. Chest x-ray to detect emphysema and rule out other lung or chest disease
6. CT scan to detect emphysema or lung cancer and analyse if a surgery is better option
7. Arterial blood gas analysers measures how well the lungs take oxygen to the blood and co2 out
8. Other laboratory test to detect the percentage of AAt in the body and rule out other conditions
Pathophysiology Of COPD
Chronic bronchitis is characterized by mucus gland hyperplasia in large airways, and by goblet cell metaplasia, chronic inflammation, and mucus plugging in small airways. Emphysema is characterized by de-structure of alveolar walls with loss of the internal surface area of the lungs.
Chronic Bronchitis
The pathological foundation for CB is due to the overproduction of mucus in response to the inflammatory signals, this is known as mucous metaplasia. In COPD patients this overproduction and hypersecretion due to the goblet cells and decreased the elimination of mucus.[1] The mechanisms responsible for mucous metaplasia in COPD patients is associated with the function of the T cells, although it is still poorly understood. It is believed to be linked to end production of the Th2 inflammation cells while the cellular response is thought to be attributed to the Th1 inflammation cells, both produce cytokines that have an influence on mucus production associated with COPD patients.
Mucus metaplasia causes airflow obstruction by several mechanisms: it causes luminal occlusion; the thickening of the epithelial layer intrudes on the airway lumen, and the mucus alters the airway surface tension. These all leave the airway at a greater risk for collapsing and decreases the capacity for airflow and gas exchange.
It was also found that smokers with moderate COPD and CB had a greater number of goblet cells in their peripheral airways, which increases the potential of mucus in the lungs. It was found that as a greater number of small airways were blocked with mucus the greater the severity of the disease.
Mucus hypersecretion is one of the risks associated with cigarette smoke exposure, viral infections, bacterial infections, or inflammatory cell activation. When combined with poor ciliary function, distal airway occlusion, ineffective cough, respiratory muscle weakness, and reduced peak expiratory flow clearing secretions is extremely difficult and requires high energy consumption.
Emphysema
The alveoli and the small distal airways are primarily affected by the disease, followed by effects in the larger airways. Elastic recoil is usually responsible for splinting the bronchioles open. However, with emphysema, the bronchioles lose their stabilizing function and therefore cause a collapse in the airways resulting in gas to be trapped distally.
There is an erosion in the alveolar septa causing there to be an enlargement of the available air space in the alveoli [4]. There is sometimes a formation of bullae with their thin walls of diminished lung tissue.
Smoking contributes to the development of the condition initially by activating the inflammatory process. The inhaled irritants cause inflammatory cells to be released from polymorphonuclear leukocytes and alveolar macrophages to move into the lungs. Inflammatory cells are known as proteolytic enzymes, which the lungs are usually protected against due to the action of antiproteases such as the alpha1-antitrypsin. However, the irritants from smoking will have an effect on the alpha1-antitrypsin, reducing its activity. Therefore emphysema develops in this situation when the production and activity of antiprotease are not sufficient to counter the harmful effects of excess protease production. A result of this is the destruction of the alveolar walls and the breakdown of elastic tissue and collagen. The loss of alveolar tissue leads to a reduction in the surface area for gas exchange, which increases the rate of blood flow through the pulmonary capillary system.
Adapted from https://www.physio-pedia.com/Emphysema
Pharmacotherapy Of COPD
In stable COPD, pharmacotherapy is used to relieve symptoms, reduce the frequency and severity of acute exacerbations, reduce disease progression and mortality, and improve health status and increase exercise tolerance.
Read Also: Treatment of pneumonia
For many years, smoking cessation has been known to be the single effective intervention for reducing the risk of developing COPD and slowing its progression down.
Bronchodilators
Drugs that relieve bronchial obstruction by reducing bronchial smooth muscle contraction are called bronchodilators. Usually, they improve spirometric values reflecting obstruction such as FEV111. These compounds generally improve also emptying of the lungs and reduce air trapping (dynamic hyperinflation/restriction) both at rest and during exercise.
The dose–response effect of all bronchodilators at the currently used doses is relatively flat, which means that a small increase (e.g. doubling) in the dose is not expected to produce a vast increase in the bronchodilatory action. The adverse effects are generally dose-related. Increase in the dose of short-acting inhaled β2-agonist and anticholinergic, especially when given nebulized, may relieve subjective dyspnoea in acute settings during an exacerbation of COPD but may not help as a long-term therapy. Bronchodilators can be divided into short acting (duration of bronchodilatory effect generally 3–6 hr) and long acting (duration of bronchodilatory effect generally 12–24 hr). There are two different classes of bronchodilators that have basically similar bronchodilatory action in the treatment of COPD but different mechanisms of action. These pharmacological classes are β2-agonists and muscarinic receptor (M1, M2 and M3) antagonists (termed anticholinergics). Both of these pharmacological classes contain short-acting and long-acting preparations.
Short And Long-acting β2-agonists (SABA, LABA)
The main beneficial effect of β2-agonists is the reduction of bronchial smooth muscle contraction that leads to relief of bronchial obstruction. The duration of the effect of short-acting β2-agonists is usually 3–6 hr. Short-acting β2-agonists are used either as-needed or regularly to reduce symptoms of COPD and improve lung function. The effect of long-acting β2-agonists lasts 12 hr (formoterol or salmeterol) or 24 hr (indacaterol, olodaterol or vilanterol). The bronchodilatory action of formoterol/indacaterol/olodaterol/vilanterol starts sooner (within 5 min.) than that of salmeterol (within 20–30 min.).
Short- and long-acting anticholinergics (SAMA, LAMA)
Anticholinergic compounds block muscarinic receptors (M1, M2 and M3), thus antagonizing acetylcholine-induced bronchial smooth muscle contraction. The duration of the effect of short-acting anticholinergic (ipratropium) is usually somewhat longer (even up to 8 hr) than that of the short-acting β2-agonists (3–6 hr), but starts more slowly 54,55. The effect of long-acting anticholinergics lasts either 12 hr (aclidinium) or approximately 24 hr (glycopyrronium, tiotropium or umeclidinium).
Combination bronchodilator Therapy
Bronchodilators with a different mechanism or duration of action can be relatively freely combined (table(table5),5), and the combination may have a better bronchodilatory effect 81. For example, combination of a short-acting anticholinergic with a short- or long-acting β2-agonist improves FEV1 better than any of the single agents.
Read Also: Allergen in school laboratory
We also have inhaled glucocorticoids, a combination of inhaled glucocorticoid and long-acting β2-agonist, oral glucocorticoids and roflumilast.
Previously, it has been conceptualized that COPD treatment should follow a stepwise approach, depending exclusively on disease severity as assessed by spirometry. Initially in mild (stage I) COPD, active risk reduction should be pursued with the addition of short-acting bronchodilators as-needed. As the disease progresses and lung function declines (stage II–IV) regular (maintenance) treatment with one or more long-acting bronchodilators, such as a long-acting muscarinic antagonist (LAMA; also known as a long-acting anticholinergic) or long-acting -agonist (LABA), should be introduced alone or in combination with ICS.
For the low exacerbation risk phenotype, pharmacotherapy with short-acting β2-agonists (salbutamol, terbutaline) or anticholinergics (ipratropium) or their combination (fenoterol–ipratropium) is recommended in patients with less symptoms. If short-acting bronchodilators are not enough to control symptoms, a long-acting β2-agonist (formoterol, indacaterol, olodaterol or salmeterol) or a long-acting anticholinergic (muscarinic receptor antagonists; aclidinium, glycopyrronium, tiotropium, umeclidinium) or their combination is recommended. For the high exacerbation risk phenotype, pharmacotherapy with a long-acting anticholinergic or a fixed combination of an inhaled glucocorticoid and a long-acting β2-agonist (budesonide–formoterol, beclomethasone dipropionate–formoterol, fluticasone propionate–salmeterol or fluticasone furoate–vilanterol) is recommended as a first choice. Other treatment options for this phenotype include combination of long-acting bronchodilators given from separate inhalers or as a fixed combination (glycopyrronium–indacaterol or umeclidinium–vilanterol) or a triple combination of an inhaled glucocorticoid, a long-acting β2-agonist and a long-acting anticholinergic. If the patient has severe-to-very severe COPD (FEV1 < 50% predicted), chronic bronchitis and frequent exacerbations despite long-acting bronchodilators, the pharmacotherapy may also include roflumilast. ACOS is a phenotype of COPD in which there are features that comply with both asthma and COPD. The treatment should cover both diseases. Generally, the therapy should include at least inhaled glucocorticoids (beclomethasone dipropionate, budesonide, ciclesonide, fluticasone furoate, fluticasone propionate or mometasone) combined with a long-acting bronchodilator (β2-agonist or anticholinergic or both). Moreover, it has been demonstrated that despite the relative steroid insensitivity of airway inflammation in COPD, the combination of long-acting bronchodilator therapy with inhaled glucocorticosteroids (ICS) is beneficial for patients with severe COPD.
Other medications include theophylline (both a bronchodilator and a phosphodiesterase inhibitor) and the phosphodiesterase-4 antagonists, such as roflumilast. Finally, a number of novel long-acting anticholinergics and β2-agonists with once or twice daily profiles are in development and clinical testing.
Non-pharmacological treatment modalities include smoking cessation 28, oxygen therapy, physical exercise and pulmonary rehabilitation, ventilator support and surgical therapy. Other date palliative care, humidifier, drink plenty of water, maintain healthy body mass index (BMI), vaccination against pneumonia especially at old age, avoid eating full (break meal into 5 times a day), clear airway an hour before meal and drink last thing after food
Adapted from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4409821/.

Comments
Post a Comment
Please have your say