Pharmacotherapy/Treatment Of Liver Cirrhosis
Liver cirrhosis is defined as scarring (fibrosis) of the liver cells and tissues. This is caused by long term liver disease. The scar tissue prevents the liver from carrying out its function properly depending on the level of damage. The scar blood bile duct. It is the end stage of any liver disease. It can eventually lead to liver failure.
 |
| Liver cirrhosis |
Symptoms Of Liver Cirrhosis
Since liver cirrhosis is the end stage of other liver disease, symptoms depend on the disease causing liver cirrhosis. As the liver gets to critical level, the following may manifest:
1. Feeling tired and weak
2. Feeling sick and nausea
3. Loss of appetite, muscle mass and weight
4. Red papules on the palm
5. Small spider web like blood vessels (spider angiomas) on the skin and above waist level
Complications Of Liver Cirrhosis
1. Jaundice
2. Vomiting blood
3. Itchy skin
4. Dark pee and tarry looking poop
5. Bleeding and bruise easily
6. Swollen legs or tummy (ascites) from fluid build-up known as portal hypertension (swelling in legs, ankles and feet)
7. Low libido.
8. Splenomegaly
9. Hepatopulmonary syndrome
10. Kidney failure
11. Confusion
12. Difficulty thinking
13. Changes in behaviour which occur due to accumulation of toxins
14. Hypersplenism
15. Infection
16. Malnutrition
12. Liver cancer
Diagnosis Of Liver Cirrhosis
1. Blood test: this test evaluates the presence or absence of some chemical and even the quantity. Normal liver releases some chemicals into the body and metabolises the others. Presence of a large quantity of chemical that is supposed to be removed from the body by the liver can indicate liver disease. Also, lower quantity of a chemical that is supposed to be released by the liver into the body indicates liver disease. For example, lower amounts of albumin and blood clotting factors indicate liver cirrhosis. Also, lower levels of liver enzymes can cause inflammation of the legs and tummy which is also a positive indication of liver cirrhosis. When the white blood cell (WBC) is high, infection is suspected. Lower levels of iron also indicate hemochromatosis, a liver disease. Reducing the number of antibodies is caused by autoimmune disorders such as autoimmune hepatitis. Others are higher creatinine and bilirubin that cause liver failure. Higher levels of alpha-1-trypsin protein causes liver cancer. Lower sodium is also another indication of liver cirrhosis.
Read Also: An Overview On The Various Types Of Hepatitis Disease
2. Ultrasound, computer topography (CT) scan and magnetic resonance imaging (MRI) are also use to evaluate liver cirrhosis
3. Transient elastography
4. Liver biopsy
5. Physical examination for things like jaundice
6. Endoscopic retrograde cholangiopancreatography use to detect bile duct problem
7. Upper endoscopy to detect enlarge veins
Cause Of Liver Cirrhosis
Common causes of cirrhosis of the liver include:
1. Alcohol: Alcohol causes a range of liver diseases, which include simple and uncomplicated fatty liver (steatosis), more serious fatty liver with inflammation (steatohepatitis or alcoholic hepatitis), and cirrhosis.
2. Nonalcoholic fatty liver disease
Cryptogenic Causes
1. Chronic viral hepatitis (A, B, and C): Chronic viral hepatitis is a condition in which hepatitis B or hepatitis C virus infects the liver for years. Most patients with viral hepatitis will not develop chronic hepatitis and cirrhosis. The majority of patients infected with hepatitis A recover completely within weeks, without developing chronic infection. In contrast, some patients infected with hepatitis B virus and most patients infected with hepatitis C virus develop chronic hepatitis, which, in turn, causes progressive liver damage and leads to cirrhosis, and, sometimes, liver cancers.
2. Autoimmune hepatitis: Autoimmune hepatitis is a liver disease found more commonly in women that is caused by an abnormality of the immune system. The abnormal immune activity in autoimmune hepatitis causes progressive inflammation and destruction of liver cells (hepatocytes), leading ultimately to cirrhosis.
3. Inherited (genetic) disorders like alpha-1-trypsin protein which is the build-up of abnormal protein in the body
4. Primary biliary cirrhosis (PCB)
5. Primary sclerosing cholangitis (PSC)
6. Infants born without bile ducts
Less common causes of cirrhosis
1. Unusual reactions to some drugs
2. Prolonged exposure to toxins
3. Chronic heart failure (cardiac cirrhosis)
4. Amyloidosis
5. Black bile duct
6. Wilson disease (excess copper)
7. Cystic fibrosis (sticky, thick mucus builds)
8. Glycogen storage disease, GSD (cannot store or breakdown glycogen properly)
9. Alagille syndrome is an inherited condition in which bile builds up in the liver because there are too few bile ducts to drain the bile.
In certain parts of the world (particularly Northern Africa), infection of the liver with a parasite (schistosomiasis) is the most common cause of liver disease and cirrhosis.
Risk Of Liver Cirrhosis
Diabetes and obesity
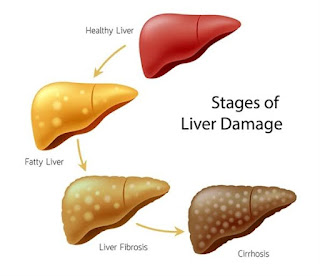
Stages Of Liver Cirrhosis
Stage 1: Compensated cirrhosis is liver Cirrhosis without symptoms
Stage 2: portal hypertension and varices
Stage 3: Decompensated cirrhosis is liver cirrhosis with symptoms
Stage 4: is referred to as end stage liver disease (ESLD)
Pathophysiology Of Liver Cirrhosis
Liver fibrosis that is accompanied by distortion of the hepatic vasculature. It leads to shunting of the portal and arterial blood supply directly into the hepatic outflow (central veins), compromising exchange between hepatic sinusoids and the adjacent liver parenchyma, i.e., hepatocytes. The hepatic sinusoids are lined by fenestrated endothelia which rest on a sheet of permeable connective tissue (the space of Disse) which contains hepatic stellate cells (HSC) and some mononuclear cells. The other side of the space of Disse is lined by hepatocytes which execute most of the known liver functions. In cirrhosis the space of Disse is filled with scar tissue and endothelial fenestrations are lost, a process termed sinusoidal capillarization.
Adapted from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2271178/
Pharmacotherapy/Treatment Of Liver Cirrhosis
There is no cure. Treatment is to prevent further damage to the liver. Treatment targets the cause of the disease, prevents symptoms and treats complications.
Read Also: Pharmacotherapy/Treatment Of Hepatitis B And Hepatitis C Virus
1. Portal hypertension: Portal hypertension is mainly the result of chronic end-stage liver disease. Treatment consists of treating its many complications. Treatments of portal hypertension include giving beta blockers or nitrates to lower blood pressure in your veins. E.g propanol and isosorbide dinitrate
2. Hepatic encephalopathy: Prescribing lactulose to absorb toxins in the blood that result from hepatic encephalopathy, which cause symptoms including confusion and other mental changes. Low protein diets also help.
3. Bacterial peritonitis: Antibiotics and infusion of a protein (albumin) will be prescribed. Typically patients are admitted to the hospital for treatment and monitoring. Following a diagnosis of bacterial peritonitis, an oral antibiotic will be prescribed for daily use to prevent recurrence of infection. A good antibiotic of choice is rifaximin which when taken does not get absorbed into the bloodstream. IV cefotaxime, norfloxacin or sulfamethoxazole and trimethoprim is given when the white blood cell (neutrophils) is above 250/cc which is an indication of spontaneous bacterial peritonitis.
4. Kidney failure: Treatment may include medication to improve kidney ability to filter waste.
5. Liver failure: Treatment depends on if you have acute or chronic failure. For chronic liver failure, diet and lifestyle changes include stopping alcohol and medications that harm the liver; eating less red meat, cheese and eggs; losing weight; controlling high blood pressure and diabetes and cutting down on salt.
Acute treatments for liver failure include intravenous fluids to maintain blood pressure, laxatives to help flush toxins from the body and blood glucose monitoring.
In summary treatments for alpha-1 antitrypsin disease include medicine to reduce swelling in the abdomen and legs. Antibiotics are used for infection. Then removal of blood is done to achieve lower iron in hemochromatosis. In Wilson disease, zinc supplement is given to prevent the absorption of copper and diuretic to remove copper, sodium and excess fluid. A good diuretic is spironolactone and furosemide. For cystic fibrosis methods to clear mucus improve lung function. Maintaining glucose at the right level improves glycogen storage disease. Ursodiol is a drug that opens narrow or blocked bile ducts. Steroids such as prednisolone and azathioprine reduce the immune system.
Surgery
The following is use in portal hypertension;
1. Cutting off blood flow through the varices to stop or reduce further bleeding with procedure using tiny elastic bands (band ligation) or with sclerotherapy.
2. Redirecting blood from the portal vein to reduce pressure in the portal vein and to control variceal bleeding. This is achieved using either one of two techniques – distal splenorenal shunt, catheter or transjugular intrahepatic portosystemic shunt (TIPS)
3. Draining excess fluid in your abdomen (ascites) in a procedure called paracentesis.
Liver Failure: If you have either acute or chronic liver failure, your liver specialist may recommend a liver transplant. Liver transplants can come from a living or deceased donor. Only a portion of the donor liver needs to be transplanted. The liver is the only human organ capable of growing back.
Read Also: Danger Of Eating Meat Tenderize With Paracetamol
Many tests are required of both you (the liver transplant recipient) and the person donating a portion of their liver or the cadaver liver (liver from a deceased person). If your doctors determine that you need a liver transplant, you will be placed on a national liver transplant waiting list, which lists patients by blood type, body size and severity of end-stage liver disease.
Liver cancer: Treatment depends on the stage of your cancer and other factors. One or more treatments may be tried. Options include surgery to remove part of your liver or your whole liver (to be replaced with a new liver as part of a liver transplantation) and nonsurgical tumor-destroying methods including ablation, chemotherapy, targeted therapy (drugs zero in on cancer genes or tissue), immunotherapy and radiation bead therapy (inject bead that give off radiation into the blood vessels that feed the tumor).
Kidney Failure: dialysis and kidney transplant depending on the cause and extent of failure. Immunomodulators are given to suppress the immune system from rejecting the donated kidney. E.g Cyclosporine (CsA) and tacrolimus (TAC) are the primary immunosuppressive drugs.
Other surgery are;
Injection sclerotherapy: a substance is injected into the varices which trigger a blood clot to form scar tissue. The scar tissue stops bleeding.
Lifestyle Modification
1. Stop drinking alcohol
2. Avoid medication that stress the liver like nonsteroidal anti-inflammatory drugs (NSAIDs) and paracetamol
3. Healthy diet especially food rich in vitamin D and K and low in protein.

Comments
Post a Comment
Please have your say