Pharmacotherapy/Treatment Of Rheumatoid Arthritis (RA) And Osteoarthritis (OA)
Arthritis is the umbrella term used to describe inflammation of joints. There are two types of arthritis. They are rheumatoid arthritis (RA) and osteoarthritis (OA). There is a third class which is juvenile idiopathic arthritis. But because there is no clear definition aside from arthritis that occurs in adolescents below the age of 17, many books don't include it.
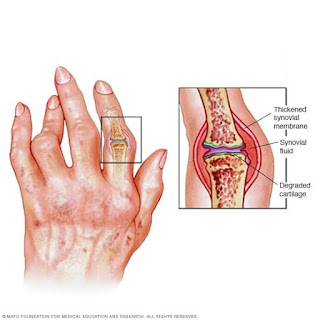 |
| Rheumatoid and osteoarthritis |
Rheumatoid Arthritis (RA)
In RA, the immune system suspects the soft lining around the joints as threats and attacks. It is just the way they attack foreign matters like bacteria and viruses. The immune system sends many fighting cells to the joint which accumulates. This leads to swelling. The swelling increases the pressure around the joints causing inflammation, stiffness and pain.
Osteoarthritis (OA)
In OA, there is loss of cartilage around the joints. This leads to a gradual degeneration of the cartilage making the bones around the joint to rub against each other. The robbing leads to inflammation and pain.
Difference Between Rheumatoid Arthritis And Osteoarthritis
Rheumatoid arthritis is an autoimmune condition why osteoarthritis is a degenerative joint condition. Rheumatoid arthritis can lead to osteoarthritis with time if not treated. Where osteoarthritis affects the weight bearing joints of the body like the kneel, hips and spine, rheumatoid arthritis affects any joint in the body almost at equal degree.
Read Also: Treating Of Body Pain In Peptic Ulcer Patient
Risk Factor (RA)
This condition occurs in both male and females but is more common in females. It can develop at any age but the risk increases in adults. It is also hereditary.
Risk Factor (OA)
This condition occurs in both male and females but is more common in females. It can develop at any age but is more common in adults. It is also hereditary and risk increases with weight. Overweight, joint deformities, diabetes, gout and history of injury to the joint increase the risk of osteoarthritis.
Symptom Of Both RA And OA
1. Pain in the joints
2. Stuff joint
3. Can't walk or run for a long time unlike before
4. Warmth or tenderness in the affected area
5. Symptoms occur in the morning
Characteristics Of RA
1. Low grade fever especially in children
2. Muscle aches
3. Excessive fatigue all over
4. Rheumatoid nodules (hard lump under the skin)
Characteristics Of OA
1. Pain occur only at joints due to friction
2. Bones may be inflamed and grow out called bone spur
3. Lumps occur under the skin close to the joints. The lump is due to the bones at the joints changing shape and getting sharp edges due to continuous friction
4. Present in kneel, hand, fingers, hips and spine
Diagnosis Of RA
1. Physical examination
2. X-ray, ultrasound and magnetic resonance imaging (MRI) to detect infection, erosion and fluid buildup
3. Increase in c-reactive protein and erythrocytes sedimentation rate (ESR) means there is inflammation. Erythrocytes will settle faster when they are inflamed and heavy.
4. Blood test to detect rheumatoid factor (RF) and anti citrullinated protein antibodies (ACPAs) which are specific markers for RA and can indicate RA.
Types Of RA
1. Seropositive people have ACPAs after blood tests. These antibodies attack the synovial fluid in the joints and produce symptoms of RA. About 60-80% of people with RA have ACPAs. For many people, ACPAs precede the symptoms of RA by 5-10 years.
2. Seronegative people are a small group of people with RA without ACPAs or RF in their blood.
Diagnosis Of OA
1. Physical examination
2. X-ray, ultrasound and MRI to detect infection, erosion and fluid buildup
3. Blood test to detect ACPAs and RF and exclude RA
Complication Of RA
1. Osteoporosis
2. Rheumatoid nodules
3. Dry eyes and mouth
4. Infection due to impaired immunity from the use of RA drugs
5. Carpal tunnel syndrome
6. Heart problems
7. Lung disease
8. Lymphoma
9. Obesity
10. Unemployment
11. Vasculitis
Complication Of OA
1. Pain around affected joints
2. Stiffness around affected joints
3. Depression
4. Sleep disturbance
Read Also: Pain Management Using Medicine Approach
Pathophysiology Of RA
Rheumatoid arthritis (RA) is a systemic inflammatory disease mainly characterized by synovitis and joint destruction. Etiology of RA is unknown. Although the impact of genetic factors is obvious, the genetic basis is not sufficient to explain the triggering of the immune insult. The dominant feature is inflammation, primarily in synovium. The synovial membrane in RA becomes hyperplastic. There is an increased number of both type synoviocytes and is infiltrated with immune and inflammatory cells: particularly macrophages, B- and T-lymphocytes, plasma cells and dendritic cells. Increased levels of cytokines are present. Cytokines play a central role in the perpetuation of synovial inflammation. The persistence of the chronic inflammatory response in conjunction with ongoing joint destruction (is found in many patients with RA despite the use of effective anti-inflammatory agents and disease-modifying drugs) probably appears as a direct result of the sustained recruitment, inappropriate retention and impaired apoptosis.
Pathophysiology of OA
In healthy joints, two bones articulate with one another separated by shock-absorbing cartilage. Both the cartilage and the bone are important in dissipating the load placed through joints every day. When joints are subjected to large loads or impact, the cartilage and bone may be damaged.
Numerous repair mechanisms attempt to restore normal function within the damaged joint to ensure the joint continues to dissipate load correctly. This includes cell-mediated remodelling within the architecture of the cartilage and subchondral bone tissues. When the rate of damage exceeds the rate of repair, degeneration of the bone and cartilage ensues and the joint fails to effectively dissipate load.
This results in a cycle of biomechanical and biochemical degeneration, where the shock-absorbing cartilage is progressively destroyed, exposing the bone to greater load and leading to bone damage (bone marrow lesions). This leads to further loss of cartilage, narrowing of the joint space (the space between the bones) and the overgrowth of bone (osteophyte formation), which causes hard lumps to develop around the joints.
Joint degeneration results in painful and tender inflammation of the synovial lining of the joint (synovitis) and swelling of the joint (effusion). While the cartilage, bone and synovial lining are important tissues, the whole joint is involved in the pathogenesis.
Modern imaging techniques, such as magnetic resonance imaging (MRI), have established that the loss of cartilage, bone marrow lesions and synovitis are common in OA and are predictive factors for requiring a joint replacement. MRI-detected synovitis and bone marrow lesions are also associated with OA pain. Synovitis may be present in early cartilage changes to the joint, and there is cellular infiltration with macrophages, activated T and B cells and accompanying vascular proliferation. Inflammatory cytokine levels may also be elevated in the joint, but to a lesser extent than seen in RA.
Pharmacotherapy/Treatment Of RA
There is no cure for rheumatoid arthritis. Available drugs and lifestyle modifications are for management and to prevent further degeneration of the joints cartilage. Treatment should be initiated immediately when it is detected as RA can get complicated within 2 years. The first class of drugs are the non steroidal antiinflammatory drugs (NSAID). These can be oral and or topical. When oral and topical NSAID are used concomitantly, the dose of the oral should be reduced. For example, the dose of oral diclofenac should be reduced when used together with topical diclofenac preparation.
NSAID tablets may be needed if paracetamol and topical NSAIDs are not easing the pain. They may not be suitable for people with certain conditions, such as asthma, a stomach ulcer or angina, or if you have had a heart attack or stroke. They should not be taken for long. If you're taking low-dose aspirin, ask your GP whether you should use a NSAID.
Paracetamol is given 1g every four hours. Diclofenac 50mg daily is recommended in minor cases. Severe cases can be increased to 75mg, 100mg or 150 mg in divided doses of 12 hours.
Steroids can also be used as they have been shown to alleviate the pain associated with RA. A good example is prednisolone given a maximum of 60 mg daily. Major side effects especially when used for a long time is to reduce immunity.
Disease modifying antirheumatic drugs (DMARDs) are the second drugs of choice in treating RA when paracetamol, NSAID and steroids fail to achieve reasonable success. A good example is hydroxychloroquine, sulfasalazine and methotrexate. They are used for up to six months.
Taking hydroxychloroquine long-term or at high doses may cause irreversible damage to the retina of your eye that could progress to permanent vision problems. The risk of retinal damage is higher in people with pre-existing eye problems, kidney disease, or people who also take tamoxifen. Hydroxychloroquine can cause dangerous effects on your heart, especially if you also use certain other medicines including the antibiotic azithromycin. Hydroxychloroquine is usually taken daily. Initial dose of 400 to 600 mg salt (310 to 465 mg base)/day orally divided in 1 or 2 doses. Maintenance dose of 200 to 400 mg salt (155 to 310 mg base)/day orally divided in 1 or 2 doses. Maximum dose is 600 mg salt (465 mg base)/day or 6.5 mg/kg salt (5 mg/kg base)/day, whichever is lower
Comments
-The action of this drug is cumulative and may require weeks to months to achieve the maximum therapeutic effect.
-When a good response is obtained, the initial dose may be reduced by 50% and continued at a maintenance dose.
-Higher incidence of retinopathy reported when this maintenance dose is exceeded; 600 mg salt (465 mg base) or 6.5 mg/kg salt (5 mg/kg base), whichever is lower, should not be exceeded per day.
-Corticosteroids and salicylates may be used with this drug, and they can generally be decreased gradually in dosage or eliminated after a maintenance dose of this drug has been achieved.
Methotrexate may cause injury or death to an unborn baby and should not be used during pregnancy to treat arthritis. Avoid having low blood cell counts, a weak immune system, alcoholism or chronic liver disease, or if you are breastfeeding. This medicine is sometimes taken only once per week, or 2 to 4 times per week. Some conditions are treated daily for just a few days followed by a rest period of 1 week or longer before taking the medicine again.
Sulfasalazine can come in delayed-release tablets and given as 1000 mg orally twice a day. The following is a Suggested dosing regimen:
1. Week 1: 500 mg orally once a day in the evening
2. Week 2: 500 mg orally twice a day (morning and evening)
3. Week 3: 500 mg orally in the morning and 1000 mg in the evening
4. Week 4: 1000 mg orally twice a day (morning and evening)
Comments
-To reduce possible GI intolerance, a lower starting dose (e.g., 0.5 to 1 g/day) is recommended; a suggested dosing regimen is provided above.
-Degree of improvement in number and extent of actively inflamed joints can be evaluated to determine efficacy of drug therapy.
-This drug does not produce an immediate response. Concomitant analgesics and/or NSAIDs are recommended (at least until the effect of this drug is evident).
-Therapeutic response has been seen 4 weeks after starting therapy; 12 weeks of therapy may be needed before clinical benefit is noticed.
-Increasing the daily dose to 3 g/day may be considered if clinical response is inadequate after 12 weeks; careful monitoring suggested for doses over 2 g/day.
Newer Antirheumatic Agent
There are newer antirheumatic agents or drugs developed for use. They are called conventional DMARDs.
Biologic agents or biologic response modifier: they are tumour necrosis factor alpha (TNF alpha) inhibitors such as Etanecef and abatacept work better with DMARDs. They prevent inflammation by suppressing TNF alpha which signals the brain to pain.
Read Also: Pharmacotherapy/Treatment Of Diabetes
Janus kinase (JAK) inhibitors belong to a family of medicines called synthetic DMARDs. Three JAK inhibitors, baricitinib (Olumiant),tofacitinib (Xeljanz), and upadacitinib (Rinvoq) may be used when others fail. Higher doses of tofacitinib may increase risk of blood clot in the lungs, serious heart related events and cancer.
Surgery
1. Synovectomy is the removal of the inflamed lining of the Joint
2. Tendon repair
3. Joint fusion
4. Total joint replacement
Lifestyle Modification
1. Exercise
2. The use of heat and cold compress
3. Assisting devices like walking stick around the house
4. Weight reduction
Alternative Supplements
Fish oil and plant oil like evening primrose and blank currant contain a certain type of fatty acid that may help with rheumatoid arthritis, pain and stiffness.
Pharmacotherapy/Treatment Of Osteoarthritis
The use of NSAID is the first line of treatment. They come in tablets, creams, spray and robb preparation. Treatment plan for minor OA is similar to that of RA. Steroid, hyaluronic acid and narcotics can be injected into the site.
Capsaicin cream is made from chilli. It works after like two weeks from regular application. It should be used for a month. It works by blocking the nerve sending pain messages in the treated area.
It should be used in small quantities at any given time four times a day. Application on sensitive and broken skin like eyes and genitals can cause some slight burning, although not severe.
Surgery
Arthroscopy, joint replacement surgery and joint fusion can be used in osteoarthritis. Transcutaneous electrical nerve stimulation uses electrical impulses through sticky patches called electrodes attached to the skin. This helps ease the pain caused by OA by numbing the nerve endings in the spinal cord which control pain.
There is another surgery done to help OA. It is osteotomy which is the adding or removal of a small section of bone either above or below knee cap or joint. This is done to shape the joints from having sharp edges due to friction.
Lifestyle Modification
Exercise, weight reduction and an adequate diet helps. Sunbathing which helps get natural vitamin D3 from the sun is also recommended.
Alternative Supplements
Glucosamine and chondroitin have been shown to receive pain but do not rebuild cartilage. Assisting devices also help. Then we have antidepressants like duloxetine that help the sufferer with depression arising from the pain. Vitamin D3 is valuable to bones and helps calcium in the body. Hot wax paraffin applied in the morning helps in changing the level of neurotransmitter responsible for pain feeling.

Comments
Post a Comment
Please have your say