Pharmacotherapy/Treatment Of Meningitis
 |
| Meningitis |
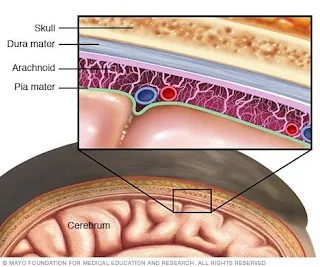
Meningitis is an infection that affects the meninges. The meninges are three fluid filled membranes covering the brain and spinal cord. Infection leads to inflammation of the meninges which is the meningitis. It begins with infection of the blood stream before the organism migrates to the meninges. It has an incubation period of about four days but some appear within 2-10 days.
Cause
It is a disease caused by bacteria, fungi, parasites, viruses and other forms of environmental conditions. The highest burden is from viruses which is less severe and in most cases resolves on its own within a week. However, bacterial meningitis is more dangerous as it can lead to death.
Virus Meningitis
Virus meningitis is responsible for about 85 percent of all meningitis. It is more common during summer and fall in the United States of America (USA). They develop as a result of cold, cold sore, flu and diarrhea. Viruses responsible for meningitis are the Coxsackie virus A and B and the echoviruses. Enteroviruses affect about 10-15 million people in a year but only a small percent develop meningitis. Others are the West Nile virus, haemophilus influenzae, mumps, human immunodeficiency virus (HIV), measles, herpes viruses and coltivirus (colorado tick fever). They are usually self limiting.
Symptoms In Infant
1. Loss of appetite
2. Irritability
3. Sleeplessness
4. Lethargy
5. Fever
6. Jaundice
7. Body or stiff neck
8. High pitch crying
9. Grumpy
10. Inconsolable behaviour
11. Difficulty walking
Symptoms In Children
1. Sudden fever
2. Body and neck ache
3. Confusion
4. Disorientation
5. Nausea and vomiting
6. Tiredness or fatigue
Symptoms In Adult
1. Headache
2. Fever
3. Stiff neck
4. Seizures
5. Photophobia
6. Sleeplessness
7. Lethargy
8. Loss of appetite
9. Nausea and vomiting
Bacterial Meningitis
They are highly contagious and disease conditions can be fatal if left untreated. It kills about 5-40 percent of children and 20-50 percent of adults infected even on treatment.
Read Also: Vaccine programme in Nigeria
Streptococcus pneumoniae causes pneumococcal meningitis and it is found in the respiratory tract, nasal cavity and sinuses. Neisseria meningitidis causes invasive meningococcal disease (IMD) such as septicemia, arthritis and meningitis and it is found in the saliva and respiratory tract. It produces the most frequent episodes of all the bacteria meningitis. It has 12 serogroups some of which are A, B, C, W, X and Y.
Staphylococcus pneumonia causes other IMD such as otitis and pneumonia. Listeria monocytogenes is a foodborne bacterial infection that can be very fatal in pregnant women. Another is staphylococcus aureus which is responsible for staphylococcal meningitis. Chronic meningitis is caused by mycobacteria. Bacterial meningitis is more common in children and prominent in sub saharan Africa.
Symptoms
1. Altered mental status
2. Nausea and vomiting
3. Photophobia
4. Irritability
5. Headache
6. Fever
7. Chill
8. Stiff neck
9. Purple areas of skin that resemble bruise
10. Lethargy
11. Sleeplessness
Pneumonia Meningitis Symptoms
1. Chills
2. Fever
3. Vomiting
4. Chest pain
5. Headache
6. Cough
7. Confusion and disorientation
8. Weakness
Meningitis rash is caused by neisseria meningitis as a late sign of infection. Meningococcal meningitis reproduce in blood and target cells around the capillary. This of course leads to damage to capillaries which cause blood to leak. This shows up as a faint pink or purple rash that looks like a tiny pin prick mistaken as a bruise. The spot grows darker and larger. These spots appear all over the body but may not be obvious in brown skin people except in the palm and inside the mouth.
Fungal Meningitis
It is a form of meningitis caused by fungi. They are rare and commonly associated with people with a weak immune system due to age, disease, drugs or other conditions e.g cancer, HIV, etc. Some are cryptococcus which is caused by inhaling air contaminated by birds dropping. Blastomyces is another form contracted from inhaling contaminated air from the soil common in Midwestern USA. Histoplasma fungi is common in areas with high populations of bats and birds, such as Mississippi River and Ohio. Coxodioldes is in the USA southwest, south and central America.
Symptoms
1. Nausea and vomiting
2. Photophobia
3. Fever
4. Headache
5. Confusion and disorientation
Parasitic Meningitis
Parasites found in food, feces and in some animals that humans eat like snails, raw fish, poultry or poultry produce can cause meningitis. The parasite or the eggs of parasites that later hatch into the parasites produce the infection. They include angiostrongylus, gnathostoma, baylisascaris, procyonis, gnathostoma spinigerum and some parasites that cause the rare type eosinophilic meningitis (EM). Amoebic meningitis is contracted in contaminated swimming water and caused by naegleria fowleri which is very deadly. Symptoms include hallucinations, seizures, and other series of symptoms.
Non Infection Meningitis
This is caused by other medical conditions or medication, lupus, head injury, brain surgery, cancer, chemical irritation, allergies, etc.
Mode Of Transmission
Since the infection meningitis normally resides in the upper respiratory tract, the major mode of transmission is through inhaling droplets of an infected person. Droplets are released after coughing, talking, laughing, sneezing, etc.
Neisseria meningitidis is in the throat at any given time. It leads to infection when it overwhelms the body's defence system. Eating contaminated food, inhaling contaminated air and certain chemical triggers can lead to meningitis.
Complications
1. Seizures
2. Hearing loss
3. Vision loss
4. Memory problem
5. Arthritis
6. Migraine and headache
7. Brain damage
8. Hydrocephalus
9. Subdural emphysema or build up of fluid between the brain and the skull
Risk Factors
1. HIV/AIDS
2. Autoimmune disorders
3. Chemotherapy
4. Bone marrow transplant
5. Living in crowded settings like dormitories, barracks, daycare, etc
6. Pregnancy
7. Children and adults above 60 years old
Diagnosis
First step in diagnosis is observation for physical symptoms such as fever, increased heart rate, neck stiffness and reduced consciousness.
The next step is a series of blood tests. Complete blood count with differential shows the level of some key parameters. In meningitis, the protein level increases, glucose level drops and the white blood cell (WBC) is elevated.
Read Also: Which is better in fighting disease? Vaccine Vs drugs
Chest x-ray is used to detect pneumonia, tuberculosis or fungal Infection. CT scan of the head reveals meningitis caused by brain abscess or sinus.
Lumbar puncture test (spinal tap) is a test that is used to determine an increase in inflammation and pressure inside the central nervous system or bacteria in the spinal fluid. Another not very sure test is the glass test that can only be done if a rash appears. A rash caused by meningitis will not fade under pressure from a glass placed on it.
Pharmacotherapy/Treatment
Drugs
Treatment plan is determined by the types of infection. The type of infection is determined through diagnosis. In some cases, treatment is initiated before laboratory analysis is out but based on symptoms. Meningitis is usually treated with intravenous (IV) antibiotics. Fungal infection is treated with an antifungal. Parasitic infections are in most cases self limiting but treatment can be initiated same also is viral infection.
In the United Kingdom, third generation cephalosporins like IV ceftriaxone and cefotaxime are the first choice for bacterial meningitis. In the USA, vancomycin can be added if there is belief there is drug resistance to cephalosporin. Chloramphenicol alone or in combination with ampicillin is also recommended especially for listeria monocytogenes.
Viral meningitis such as herpes and varicella can be treated with IV acyclovir. Cryptococcus meningitis which is caused by fungal can be treated with amphotericin B and flucytosine.
Supporting therapy with corticosteroids and painkillers such as dexamethasone and paracetamol to reduce inflammation and pain. Lumbar puncture or drain to drain sinuses. Anticonvulsant such as phenobarbital is given for patients experiencing seizures. Oxygen or ventilator for assisted breathing in severe cases. IV fluids can be administered when there is evidence to believe the patient is dehydrated and sedatives is given when rest is fine.
Vaccine
It is better to prevent than to treat. Meningococcal meningitis can be prevented with rifampicin, ciprofloxacin or ceftriaxone IV. But the best form of prevention that lasts more is the use of vaccines. The vaccines contain antigens -- substances that trigger the body's immune system and cause it to make antibodies. These antibodies then protect the body by attacking and killing the bacteria if it should invade your system. Unfortunately, vaccines currently available are only for certain types of infection. There are four vaccine licenses in the USA. Available vaccines are meningococcal conjugate vaccine (MenACWY or MCV4) approved 2015 which is responsible for prevention of four of the most common types of bacteria serogroup. It is given to teens at 11 years and a booster dose at 18. It can be given earlier if there is risk of infection to children from 2 years due to weakened immune systems. Adults above 18 can also be given if there is a risk but not suitable for people above 55 years of age. One type of MCV4, Menveo, is licensed for use in people aged 2 to 55. Another version, Menactra, is approved for those 9 months to 55 years old.
In 2015, two serogroup B vaccines were given approval and protection against the other two forms of meningococcal disease. MenB-FHpb or Trumenba was approved for a three dose schedule, while MenB-4C Bexsero is approved for two doses. Both vaccines have proven effective is protecting those aged 10-25, but have also been found to be useful for older patients. Meningococcal conjugate vaccine has a longer duration of action than MenB. MenB is not recommended for everyone. Side effects include soreness, redness and burning at the injection site. Fever, chills, fatigue, joint pain and headache are also possible.
Meningococcal polysaccharide vaccine 4 (MPSV4) is the first quadruplet vaccine approved in 1978. It is given at the age of 16. Teens with HIV will need three shots if the vaccine with about eight weeks interval between first doses and a booster shot after five years. Vaccines last for five years. Adults can also be given at the discretion of the prescriber. MPSV4 is the only vaccine licensed for use in people over 55 as well as people 2 to 55. The MCV4, MPSV4 and MenB vaccines are about 85-90% effective in preventing meningococcal disease.
Pneumococcal vaccines are vaccines against the bacterium Streptococcus pneumoniae. Their use can prevent some cases of pneumonia, meningitis, and sepsis. There are two types of pneumococcal vaccines: Pneumococcal conjugate vaccine (PCV13) and pneumococcal polysaccharide vaccine (PPSV23). They are given by injection either into a muscle or just under the skin.
PPSV23 protects against 23 types of pneumococcal bacteria while PCV13 protects against 13 types. PCV13 requires four doses. This vaccine helps prevent invasive infections like meningitis and bacteremia.
Vaccines should be considered in pregnant women, people living in dormitories, common people living in barracks, certain people that have had certain types of surgery (spleen) or on some therapy (chemotherapy). Very ill persons should not be vaccinated until they have recovered. However, vaccines can be administered to those who are experiencing mild illness. The newer vaccine should not be given to pregnant women because much information is not yet available on them.
Vaccines against some other forms of infection can also prevent meningitis. An example is Baccille Calmette-Guérin (BCG) vaccines against tuberculosis.

Comments
Post a Comment
Please have your say